Fluoroscopy-Guided Snare Retrieval of the Celt ACD Metallic Vascular Closure Device Following Failed Deployment
Abstract
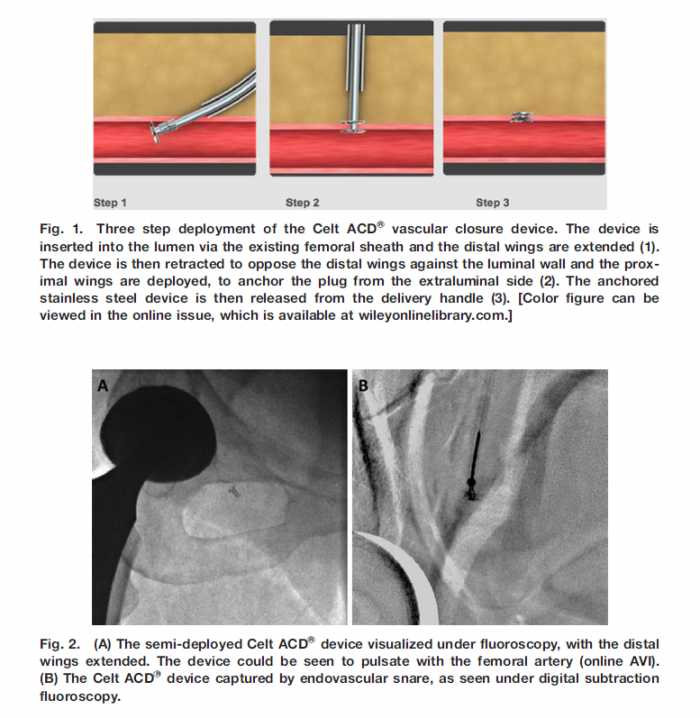
We report a case of endovascular snare retrieval of a new stainless steel vascular closure devIce (Celt CDVR , Kimal, Middlesex, UK) from the common femoral artery, following de-vice failure after diagnostic coronary angiography. The stainless steel composition of the device aided successful fluoroscopic localization and removal.
Conclusion
In this case of vascular closure device malfunction, fluoroscopic visualization of the stainless steel Celt ACDVR allowed immediate and straightforward endo-vascular retrieval without the need for surgical inter-vention.
CELT Jost Kouri Article
Patient fully anticoagulated and Closed with a CELT Device
Patient ambulated immediately and had bowel movement
Patient returned to procedure room and was successfully re-accessed at same puncture site and closed again with a second Celt device at the end of the procedure
Summary:
Modern vascular closure devices (VCDs) like the Angioseal (Terumo; Tokyo, Japan) and Celt (Vasorum Ltd; Dublin, Ireland) offer rapid mechanical hemostasis of fem- oral arterial access sites. We recount a case wherein a Celt VCD was rigorously challenged to maintain hemostasis immediately after placement due to extenuating circum- stances. The observed lack of consequent vascular compli- cations provokes curiosity about held perceptions regarding achievement of hemostasis and time to ambulation follow- ing VCD placement for percutaneous femoral access.
A 70-year-old man with a history of hepatocellular carcinoma presented for planning hepatic angiography preceding repeat radioembolization. Given his history of recurrent deep vein thromboses, the patient was chroni- cally anticoagulated on 5 mg Apixaban twice daily. It was strongly felt by his oncologist that anticoagulation should not be stopped for this procedure. Of note, pharmacologic anticoagulation was not discontinued for his previous planning angiogram or subsequent radioembolization. In both of those cases, the femoral access site was success- fully closed with an Angioseal VCD (Terumo) without incident or complication.
Early in the angiography procedure, the patient’s blood pressure was noted to rise precipitously with systolic values reaching >190 mmHg. His blood pressure did not improve despite intravenous administration of 10 mg Hydralazine. It became evident that he was expending significant abdomin- opelvic effort in response to an urgent need to void. He declined usage of a bedpan and instead indicated strong pref- erence to use a conventional bathroom near the angiography suite. The patient could not be compelled to reconsider this decision despite multiple attempts. Because arterial access had already been achieved, placement of a VCD was consid- ered. Given the team’s capacity for continuous monitoring and the patient’s close proximity to the procedural suite, the treatment team felt confident that potential complications associated with closure device failure could be effectively managed if necessary. A Celt VCD was deployed at the puncture site, and hemostasis was confirmed.

celt_retrieval
Objectives:
The Celt ACD® (Vasorum, Dublin, Ireland.) is a novel stainless steel vascular closure device (VCD). We conducted a prospective, non-randomised study to assess time to hemostasis, patient discomfort and vascular complications when using the Celt ACD® compared with both manual compression and Angio-Seal™ VIP (St Jude Medical, Minnesota, USA), the most commonly used VCD in the U.K.
Background:
150 patients undergoing elective diagnostic coronary angiography via the femoral route in our centre underwent closure of the arteriotomy using either the Celt ACD (50 patients), Angio-Seal (50 patients), or manual compression (MC, 50 patients).The choice of closure method was at the discretion of the operator. The time to deployment, time to hemostasis (total cessation of bleeding) and patient-rated discomfort were recorded. At one week following the procedure patients were contacted to assess the incidence and severity of bruising (recorded if size > 10 pence coin), and vascular complications, (pseudo-aneurysm, vascular occlusion).
Results:
The mean age (62, 59, 64 years), weight (83, 85, 85 kg) and number taking antiplatelets (27, 30, 31) or anticoagulants (7, 2, 5) was not significantly different between groups (Celt, Angio-Seal and MC respectively). In the Celt and Angio-Seal groups, VCD deployment was technically successful in all patients, and hemostasis was achieved immediately after release of the VCD in 47/50 (94%) patients in both groups. The remaining three patients in each group had minor oozing of blood requiring additional manual compression for up to 5 min (Celt) and 15 min (Angio-Seal).The mean time to deploy the device was significantly shorter for Celt compared with Angio-Seal (58 ± 6 vs 70 ± 3 seconds, p < 0.01).In the MC group, 43/50 (86%) patients had complete hemostasis after 10 min’ compression, the remainder having ongoing ooze requiring further pressure for 0.75–35 min.
Patient-rated discomfort (from 0 to 10, 10 being the most intense pain) was 1.7 ± 0.3 for MC, 2.0 ± 0.3 for Celt, and 3.3 ± 0.4 for Angio-Seal.142/150 (95%) of patients were contactable at one week post-procedure: of these significantly fewer reported minor bruising in the Celt group (12/48; 25%) compared with 30/48 (63%) for Angio-Seal and 30/46 (65%) for MC. In the VCD groups, no patient had a major vascular complication and or required medical review or further vascular imaging. In the MC group, one patient required a Doppler ultrasound for suspected pseudo-aneurysm (that proved to be normal) and another two sought medical advice due to major bruising.
Conclusions:
The Celt ACD® is associated with significantly reduced time to hemostasis, reduced patient discomfort and a lower incidence of late minor bruising compared with Angio-Seal™ VIP. A registry data on a much larger population is required to compare the incidence of major vascular complications and cost effectiveness of these two VCDs.
CeltACD_Neuro2017
Abstract
Treatment of bifurcation intracranial aneurysms is technically challenging. Sometimes it is necessary to pass a microcatheter through the aneurysm sac to navigate the microcatheter to a branch originating from the aneurysm sac. A 56-year-old male patient was treated for an incidental middle cerebral artery aneurysm. One branch originated from the medial part of the aneurysm sac, therefore stent-assisted coiling technique with an Atlas stent was used for endovascular treatment. After placementof the stent into the M2 branch, the loop of the microcatheter located in the aneurysm sac was pulled back and the microcatheter was straightened and finally the stent was deployed carefully from the M2 segment across the aneurysm sac into the M1 segment of the left middle cerebral artery. Immediately after placement of the stent the microcatheter was positioned easily through the implanted stent by crossing technique and coiling of the intracranial aneurysm was performed in the same session. No reperfusion was found on the 12-month follow-up magnetic resonance angiogram, and no clinical problem occurred during this period.
